Introduction to the Iridotomy procedure
There are certain eye conditions whereby aqueous fluid becomes trapped behind the iris and therefore, cannot follow its necessary path from the ciliary body, around the lens, through the pupil and to the drainage area of the trabecular meshwork. The normal path of aqueous flow is shown in Fig 1 below.
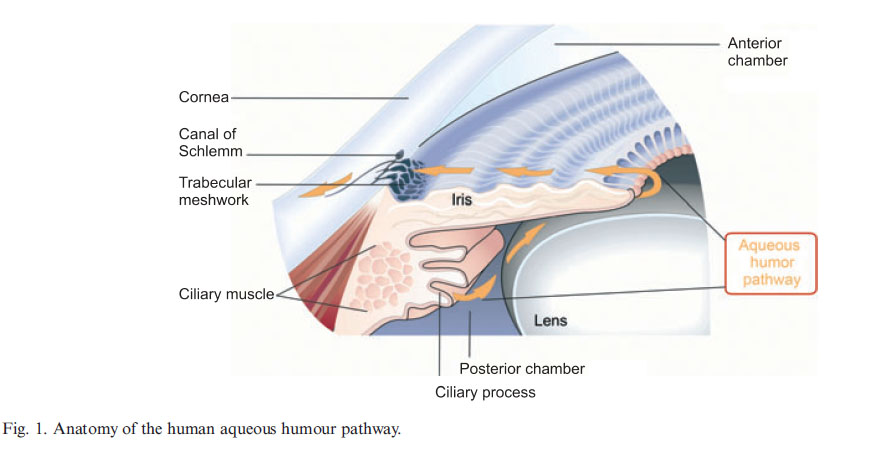
In the case of angle closure or pupillary block, there can be a partial or total blockage of fluid behind the iris, and the resulting pressure pushes the iris forward causing the angle between it and the cornea to narrow. This bulge can also cause the inside edge of the iris at the pupil to bend inward folding it towards the lens and causing pupilary block. So the goal of the iridotomy procedure is to burn a small hole with a laser through the iris so that essentially, a new pupil is formed which allows aqueous fluid another route in its flow towards the Trabecular meshwork.
In addition to being used in cases of
angle closure or pupilary block,
the iridotomy procedure is also sometimes used in pigmentary
glaucoma. However, the goal in this case is slightly different than in closed or narrow angles, and consists of relieving pressure in front of the iris by letting aqueous fluid travel in reverse, so the iris does not come in such close contact with the lens. This helps prevent pigment from being rubbed off and liberated into the drain.
Procedure description
Iridotomy is performed with either an argon laser or a neodymium:yttrium-aluminum-garnet (Nd:YAG) laser, or, in certain circumstances, with both. Before the procedure, the eyes are treated with topical proparacaine, pilocarpine 1%, and either apraclonidine (0.5% or 1%) or brimonidine (0.1%, 0.15%, or 0.2%); the use of apraclonidine or brimonidine significantly reduces the risk of postlaser intraocular pressure spike, a common complication of laser trabeculoplasty. Pilocarpine is used to stretch the peripheral iris, making it thinner and easier to penetrate. However higher concentrations of pilocarpine may cause paradoxical angle closure, so it is never recommended.
The placement of a contact lens on the other hand, makes the procedure easier as it allows the laser energy to be concentrated at the level of the iris and it also acts as a speculum, keeping the eye open to minimize fine eye movements.
The iris can be thick in patients with dark brown irises. To prevent complications such as significant pigment dispersion, iris bleeding ,and hyphema, the iris stroma is initially thinned with the argon laser, and the iris pigment epithelium is penetrated with the Nd:YAG laser.
A transient increase in intraocular pressure lasting less than 24 hours is the most common complication after the procedure. Therefore, a drop of topical apraclonidine (0.5% or 1%) or brimonidine (0.1%, 0.15%, or 0.2%) is placed on the eye before laser trabeculoplasty. Anterior segment inflammation is another common complication, also known as anterior uveitis. Bleeding is common with the use of Nd:YAG laser because it is a photo disruptive device. Bleeding, on the other hand, is uncommon with the argon laser, which causes photocoagulation.
If the iridotomy site is too close to the pupil, lens opacities can develop. Cataract formation is attributable to heat buildup during argon laser use and direct tissue disruption during Nd:YAG laser use. Also, transient blurred vision may occur in the immediate post laser period. Possible causes include pigment dispersion, inflammation, and retained methylcellulose from contact lens placement. Focal or generalized edema may also occur after argon laser peripheral iridotomy.
References:
Argon Laser Peripheral Iridotomies in the Treatment of Primary Angle Closure Glaucoma
Laser Peripheral Iridotomy (LPI)
Glaucoma Laser Treatment: Laser Peripheral Iridotomy
Peripheral Iridotomy

